It always happens in ordinary moments.
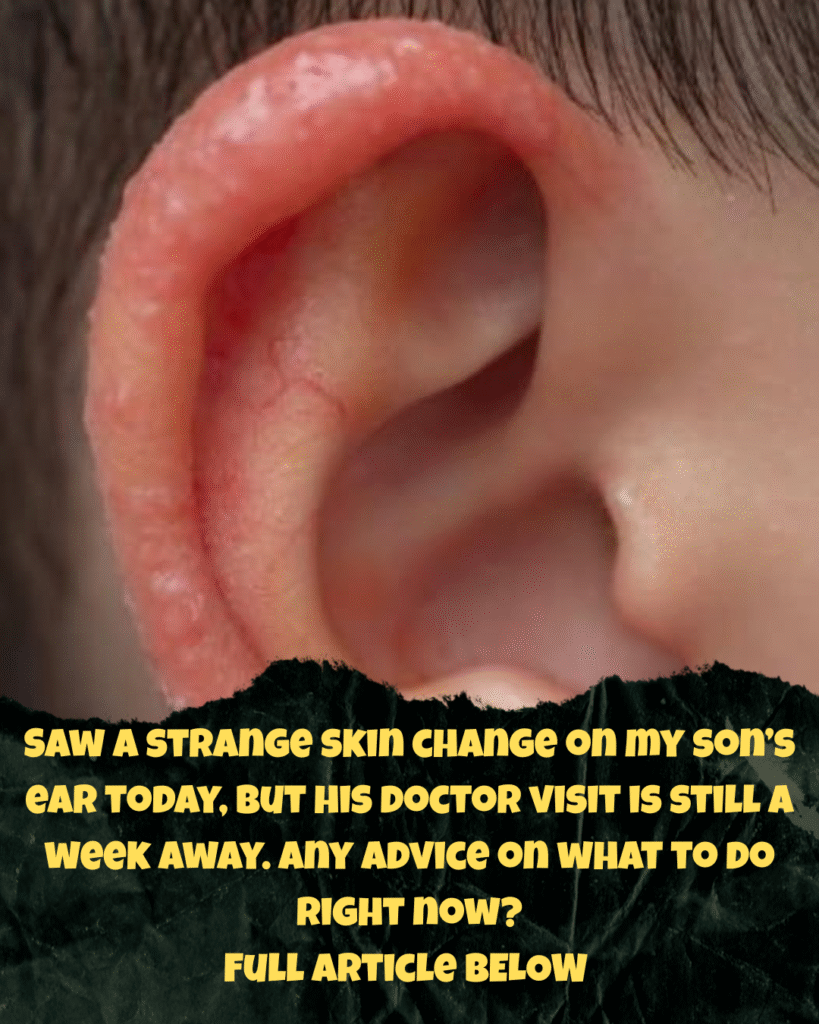
A morning sunbeam lands just right, and suddenly you notice something on your child—a mark, a patch, a color you’ve never seen before. Your breath catches. Your heart pulls tight. You lean in closer, tracing the shape of it with your eyes, wondering how long it’s been there and why you didn’t see it sooner.
Your mind rushes ahead:
Is it serious?
Is he uncomfortable?
Should I call someone now?
Should we go to urgent care?
This worry is not weakness.
It’s love, wearing a worried face.
And here’s the truth most parents don’t hear enough:
Most new patches of skin on a child’s ear are not emergencies.
And while you wait for your doctor’s appointment, there is much you can do—practical steps, calming steps, grounding steps—to support both your child’s skin and your own peace of mind.
Let’s walk this path gently, together.
What That Patch Might Be: A Soft Introduction to Childhood Eczema
One of the most common causes of new skin patches on children—especially on ears—is eczema, also known as atopic dermatitis. It affects nearly 1 in 5 children, and it tends to show up on places with thin, delicate skin.
The ear is a perfect storm of irritants:
wind, cold, friction from sleeping, soap residue, rough towels, even hair products.
What eczema often looks like:
- Pink or red patches
- Rough, dry, scaly, or thickened skin
- Tiny bumps that sometimes ooze clear fluid when irritated
- Skin that feels warm or looks slightly swollen
- Itching, scratching, rubbing (especially on your shoulder or chest when you’re holding him)
Eczema can flare suddenly and disappear slowly. It can come and go in cycles.
It is not contagious.
It is not caused by anything you did wrong.
Eczema often appears in families where someone has eczema, asthma, or allergies—but it can show up in children with no family history too.
Your First Steps: Gentle, Calming Care You Can Begin Today
While you wait for the doctor’s appointment, you are not powerless.
These simple practices soothe irritation, protect the skin barrier, and prevent the patch from worsening.
Let’s begin softly.
1. Cleanse With Tenderness (Once Per Day Only)
Your child’s skin doesn’t need scrubbing—it needs protection.
What to do:
- Wash the area once daily
- Use lukewarm water
- Choose a fragrance-free, hypoallergenic cleanser
(Examples: Cetaphil, Vanicream, CeraVe) - Pat dry with a soft towel—never rub
Avoid:
- Bubble baths
- Scented soaps
- Washcloth friction
- Hot water
Anything that strips natural oils will worsen irritation.
2. Reduce the Itch Before It Starts
Children often scratch without realizing it, especially during sleep. This can break the skin and create an infection.
Soothing, safe ways to calm itchiness:
- Cool compress
Dip a clean cloth in cool water, wring gently, hold to the ear for 1–2 minutes. - Trim fingernails
Smooth edges to prevent accidental scratches. - Soft distraction
A cold spoon held to the ear, a storybook, a cuddle—anything that shifts focus.
Avoid hydrocortisone just yet unless needed (see below). Many irritations calm down once moisture and gentleness return.
3. Moisturize Like You’re Building a Shield
Eczema loves dryness.
Moisture is your first line of defense.
What to apply:
- A thick, fragrance-free ointment such as:
- Petroleum jelly
- Aquaphor
- CeraVe Healing Ointment
- Apply immediately after bathing while skin is still slightly damp.
- Reapply 2–3 times a day.
Avoid:
- Coconut oil (can sting broken skin)
- Essential oils
- Lotions with perfumes or dyes
The ear is delicate—think protection, not experimentation.
4. Over-the-Counter Help (Used Sparingly and Wisely)
If the patch is very red or itchy, 1% hydrocortisone cream can help calm inflammation.
But:
- Use a pea-sized amount
- Apply only on the affected area
- Use once or twice daily
- No more than 3 days in a row
- Stop immediately if the skin breaks or becomes wet/oozing
Do not use hydrocortisone:
- Near the eyes
- On open wounds
- On large areas of skin
- Without checking with a doctor if your child is under 2
Skip antihistamine creams—they often irritate sensitive skin even more.
When to Call the Doctor Sooner (Red Flags to Watch For)
Most rashes can wait. But some changes need a quicker evaluation.
Call your pediatrician today if you notice:
- Yellow crust or pus (sign of infection)
- Skin that is hot to the touch
- A rapidly spreading rash
- Fever over 100.4°F (38°C)
- Swelling that blocks the ear canal
- Red streaks moving outward from the patch
Go to urgent care if:
- Your child is crying from pain
- The swelling is affecting hearing or eating
- You see blisters filled with fluid
- Your child appears lethargic or uninterested in usual activities
Your intuition matters.
If something feels deeply wrong, trust that instinct and seek care.
Preparing for Your Doctor Appointment: Your Quiet Superpower
You may feel like you're “just waiting,” but you are actually gathering valuable information that will help your child’s doctor make the right diagnosis.
Here’s what makes a difference:
1. Keep a Simple Skin Log
Write down short notes once a day:
Mon AM
Red patch behind left ear
Used cool compress + moisturizer
Less scratching before nap
This helps track patterns and triggers.
2. Take Photos
Take one clear picture each morning in the same lighting.
In one week, these photos tell a full story.
Doctors love this—you’re giving them data, not guesswork.
3. Gather Clues
Write down:
- Any new soaps, shampoos, or lotions
- Recent foods your child tried
- Laundry detergents used
- Exposure to cold, wind, chlorine, or pets
- Family history of eczema, pollen allergies, or asthma
Even small details matter.
4. Bring Questions
Clear communication helps you leave the appointment feeling empowered.
Ask your doctor:
- Is this eczema or something else?
- Should we use a medicated cream?
- What should we avoid at home?
- How can we reduce flare-ups long-term?
- When should I be concerned?
You deserve answers that feel grounding, not overwhelming.
Supporting Healing at Home: Gentle Prevention After the Flare
Once the patch improves, you can help prevent future flare-ups with small shifts.
These aren’t strict rules—they’re invitations to protect tender skin.
Laundry With Love
Use:
- Fragrance-free detergents
(“Free & Clear” options) - No fabric softeners
- A second rinse cycle to remove residue
Synthetic fragrances are a top trigger for sensitive skin.
Dress for Comfort
- Soft, breathable cotton
- No scratchy tags
- Avoid wool or rough fabrics
- A light hat or ear cover in cold weather
Ears chafe easily from wind and friction.
Bathing Wisely
- Short baths (5–7 minutes)
- Lukewarm water
- No scrubbing
- Moisturize immediately after patting dry
Hot water strips natural oils and triggers flare-ups.
Nourish From the Inside
Some children’s skin improves with:
- Hydration throughout the day
- Omega-3-rich foods
(salmon, chia, walnuts, flax) - Balanced meals with fruits and vegetables
Healthy skin is built from the inside out.
A Parent’s Heart: The Hardest Part Is the Waiting
The week before a doctor’s appointment can feel long.
You watch the patch.
You check it again.
You wonder if it’s better or worse.
You hope you're doing enough.
Here is a truth for your heart:
You are not failing him by waiting a few days.
You are not overreacting by paying attention.
You are not imagining things—you’re observing with love.
Most childhood skin changes are temporary conversations between body and environment. They are not verdicts. They do not mean danger. They simply ask for gentleness, patience, and awareness.
And you are already offering all three.
A Closing Blessing For the Waiting Days
This patch on your son’s ear is not a threat.
It’s a whisper.
A message from his skin that says:
“Something needs a softer touch.”
So while you wait for the doctor, remember:
- You are not alone.
- You are not powerless.
- You are already doing enough.
- Your child feels your calm more than your worry.
- Healing often begins with simple acts:
cool cloths, soft hands, clean water, and steady presence.
Place your hand gently on your child’s back.
Feel the rise and fall of his breath.
That is your anchor.


Leave a Reply